If there’s any two drugs that will take the world by storm for the current decade, it’s going to be the weight loss peptides Semaglutide and Tirzepatide.
In fact, Semaglutide is projected to make up $7 billion of the projected $30 billion in global sales of obesity drugs in 2030.
And given obesity’s exponentially-rising presence in the world, perhaps it’s one of the few times in history where “Big Pharma” is doing the right thing.
But there seems to be a brewing war between two factions within the health optimization space.
While individuals like myself are ecstatic at the arrival of Semaglutide and its likely successors for even faster and safer weight loss (such as Retatrutide), others are sticking firmly with their anti-pharmaceutical roots.
The people in the latter group complain about things such as current short-term side effects, unknown long-term side effects, lack of meaningful efficacy, and the exorbitant costs of Semaglutide.
So who’s right in this situation?
Are the anti “Big Pharma” folks right in their views, or are they unintentionally spreading alarmist talking points due to the misinformation fed to them by mainstream media?
I had the chance to sit down and talk with hormone specialist Dr. Rudolph Eberwein of the Medical Health Institute (MHI) clinic, who has an extensive 17-year history of working with Semaglutide and its predecessors across thousands of overweight and obese patients.

He was one of the very first physicians to start using GLP-1 agonist drugs in his clinic, and has directly observed every effect under the sun for far longer than most doctors have.
If there’s anybody who knows what’s really going on and what to look out for in the wacky world of weight loss, it’s Dr. Eberwein.
Let’s hear what he has to say!
Table of Contents
ToggleCleaning House: What You MUST Know About Semaglutide and Tirzepatide

Before we get into Dr. Eberwein’s insights, let’s make sure you’re caught up to speed on what we’re talking about.
If you don’t know anything about Semaglutide, make sure you read our introductory article on what Semaglutide is and how it works.
And if you don’t know anything about Tirzepatide, go here to get educated.
There’s a lot of information in those articles explaining the different brand names, how these drugs work in the body, and why I’m so incredibly bullish on them.
You WILL NOT understand anything I’m talking about in this article without reading those two pieces I’ve published, so please take the time to read them if this is your first time hearing about either peptide.
Once you have that sorted, make sure to read my follow-up articles on why Semaglutide and Tirzepatide are the best peptides for weight loss, a critical part of the best peptide stacks for muscle growth and fat loss, and now an integral part of my peptide stack for fully optimized living.
NOTE: From here on out, Dr. Eberwein is taking over this article.
Myth #1: Semaglutide Is “Big Pharma” Profiting From the COVID-19 Pandemic

I’ve seen a lot of anger about what the COVID-19 lockdowns have done to people’s health, and a lot of the blame being placed on pharmaceutical companies raking in unprecedented amounts of money as a result.
Most of it is justified and comes from the right place.
However, perspectives like the ones below that paint Semaglutide as the “enemy” are sorely missing some much-needed context.
I told you so... for a year after they fattened up the country with lockdowns, closing gyms and doordash while normalizing obesity praising obese models on magazine covers I told you the elites would cash in on the fattened cows with weight loss drugs and surgeries.#Nomorbidity https://t.co/9YDDvozpXe pic.twitter.com/lpSaj4vsrw
— Alan Roberts (@TheMFingCOO) January 9, 2023
Is it a coincidence that Semaglutide got approved for chronic weight management in June 2021… just as the economy was opening up and researchers were only beginning to understand the catastrophic effects of extended at-home isolation on our health?
I would say YES and there’s a very good reason why.
If you are deep in the trenches of the weight loss industry, the concept of targeting GLP-1 (glucagon-like peptide 1) is nothing new.
The discovery of GLP-1 dates all the way back to the 1980s, when researchers discovered the peptide hormone played a pivotal role in reducing blood sugar and inhibiting glucagon release by increasing insulin production.
By the 1990s, it was believed GLP-1 could “account for up to 70% of insulin secretion in response to nutrient intake” (Source).
Combined with delayed gastric emptying for an extended feeling of satiety, GLP-1 became a very promising therapeutic target for treating type 2 diabetes.
The very first GLP-1 receptor agonist (RA) to take this approach and receive full FDA approval was Exenatide, which got the stamp of approval in 2005:

(Source)
Pharmaceutical companies got better at improving these drugs in numerous ways:
- Extended half-life
- Fewer side effects
- Larger improvements of critical biomarkers for health
- Better weight loss
The last point is especially important because while clinical trials did see some weight loss and reduced hunger as a notable side effect, it wasn’t until the arrival of Semaglutide that the observed weight loss in diabetics was significant.
(NOTE: If you want to go deeper into the development of GLP-1 receptor agonists and how each successor improved upon its predecessor, go here. For an extensive history of GLP-1 itself, go here).
Coming back to my own experience with GLP-1 RAs, I have had 17 years of experience with using these drugs for diabetic patients. And this was back when nobody in my field even had a single thought to use them for chronic weight management.
And of those 17 years, the past 5 years were spent specifically using them for weight loss in patients.
There are LOTS of tips and techniques for successfully using Semaglutide and Tirzepatide that you can only learn from direct clinical experience and will not find in studies (some of which I will share in this article).
But I can confidently say we have never had effective tools like Semaglutide so freely available at our disposal, and there’s many more exciting things to come forward with its hopeful successors.
No better time in history exists to be a metabolic health doctor in the functional medicine space than right now!
In fact, internists like myself are unfortunately all too familiar with what USED to be taught in medical school as the standard of care for diabetes: Exogenous insulin or sulfonylureas.
And we’re only just finding out in recent times that both lines of treatment are tied to an increased risk of cardiovascular disease:
“…the team found patients who take one of these two drugs are more likely-36 percent more for sulfonylureas and twice as likely for basal insulin—to experience cardiovascular harm than those taking a newer class of diabetes drugs known as DPP-4 inhibitors.
According to our findings, doctors only have to prescribe basal insulin to 37 people over two years to observe one cardiovascular event, such as a heart attack, stroke, heart failure, or amputation
For sulfonylureas, that number was a bit higher—103 people. But when these numbers are applied to 30 million Americans with diabetes, this has staggering implications for how it may be harming many patients.”
I would even go as far as to argue that thanks to GLP-1 RAs evolving into the new and improved standard of care for type 2 diabetes, there is so much money to be made with these drugs that insulin prices are falling down.
Literally, as I’m writing this article, Eli Lilly just announced a dramatic 70% reduction in price for its insulin products (in case you’re unaware, they’re the same pharmaceutical company that manufactures Tirzepatide)!
And going back to Tirzepatide… while there aren’t any GLP-1 receptors on fat cells, there are indeed GIP (Glucose-dependent insulinotropic polypeptide) receptors on these fat cells.
Emerging evidence (here and here) suggests GIP is involved in lipolysis (i.e. fat burning) that is independent of caloric intake.
The important point I want to push is this: GLP-1 has been a target of interest for decades, drugs targeting GLP-1 have been in the works for 20+ years, and they have been used successfully on multiple millions of diabetic patients.
Insulin Resistance: The Root of All Chronic Illness
As a side note, I want to mention that insulin resistance is the #1 thing we seek to treat in the functional medicine world.
Especially since more evidence shows it is connected to a wide array of severe diseases:
“Epidemiological research associates insulin resistance in the etiology of these diseases, but there is limited evidence for the mechanism of damage. Emerging research suggests that hyperinsulinemia, a symptom of insulin resistance, may cause these pathological changes, and therefore be an independent contributor to these diseases.
This review shows that hyperinsulinemia, or excessive insulin secretion, should be considered independently to insulin resistance, defined as glucose uptake rate, even though the two conditions are intertwined and will co-exist under normal conditions.
Hyperinsulinemia directly and indirectly contributes to a vast array of metabolic diseases including all inflammatory conditions, all vascular diseases, gestational and type 2 diabetes, non-alcoholic fatty liver disease, obesity and certain cancers and dementias”
And the best approach is to tackle insulin resistance from numerous angles – reduction of blood sugar, restoration of normal insulin sensitivity, elimination of body fat, etc.
Tirzepatide is the best thing to happen to us because one drug can tackle several important mechanisms of action at once (alongside healthy lifestyle habits, of course).
With this history lesson out of the way, let’s tackle some other popular myths about Semaglutide.
Myth #2: Semaglutide Makes You Lose Muscle Mass

This talking point wasn’t very prominent until just last week, thanks to an article published by Dr. Peter Attia.
Dr. Attia pointed out that in two separate clinical trials for Semaglutide, roughly 40% of the total weight loss experienced by patients on the drug was lean mass.
Correctly, he explains why this can be problematic:
“…even for those with obesity, not all weight loss is healthy. While shedding excess fat mass (and in particular, visceral fat mass) has a multitude of beneficial effects on health, shedding lean mass – which includes muscle and bone – is associated with poorer health trajectories and reduced lifespan.
Therefore, safe and effective obesity treatments are those which significantly reduce fat mass while minimizing the concurrent loss of lean mass.
Though a certain amount of lean loss is inevitable with significant weight reduction (usually about 25% of total weight loss), the goal is to increase the body’s overall proportion of lean mass – in other words, to improve body composition.”
The unfortunate reality about rapid weight loss is you can’t have 100% control over WHAT you lose.
A lot of my obese patients are prone to losing muscle mass, and that’s why you cannot rely on Semaglutide or any weight loss drug alone — they are powerful tools but they are not the whole answer.
Because any veteran dieter will tell you about the paradox of how people become “fatter” despite losing weight: If you’re losing muscle alongside fat, the scale may go down but your overall fat-to-muscle ratio skews heavily towards fat.
Ironically, the answer to this dilemma is buried near the end of Dr. Attia’s article:
“Increasing weight-bearing exercise and strength training can help to counteract losses in muscle and bone mass while taking these drugs, and patients should be careful that they’re consuming sufficient protein in spite of the overall reductions in appetite and calorie intake.”
(JAY’S NOTE: I have my own gripes with Dr. Attia due to his misinformed stance on avoiding Metformin use in active people.
But as I say in my private inner circle, NO SHIT SHERLOCK!)
I do the same thing with my patients: High protein diet, resistance training, amino acid supplementation, optimized mindset, and even a correction of hormonal imbalances are all part of building and preserving lean muscle while losing weight.
You NEED those healthy lifestyle habits in place from the start of any weight loss program, otherwise you’ll end up like the high percentage of patients on gastric bypass surgery who regain their weight because absolutely nothing else was done.
Furthermore, you also need to factor in the “Set Point Theory” of weight loss and gain:
“Set point theory, as it pertains to human body weight, states that there is a biological control method in humans that actively regulates weight towards a predetermined set weight for each individual.
This may occur through regulation of energy intake (e.g.via increased or decreased appetite) or energy expenditure (e.g. via reduced metabolism or feelings of lethargy).
Set point theory explains why it is difficult for dieters to maintain weight loss over time, as calorie restriction may become less effective or more difficult to maintain as regulatory mechanisms in the body actively push the body back towards the set point weight”
As you lose weight, your hunger hormones leptin (lowers appetite) and ghrelin (increases appetite) start to become unbalanced and your body wants to “fight” back in the form of increased calorie intake and weight regain.
If you do not maintain a fully optimized lifestyle during AND after the use of Semaglutide/Tirzepatide, you will go back to your original weight.
I’ve even seen some people who gain so much visceral fat to the point of no return, where their hormonal health is so disregulated that they will always bounce back to their starting weight no matter how long or hard they diet.
And you don’t even need to maintain a 100% hardcore dieter lifestyle once you reach your target weight and stop using Semaglutide — following the 80/20 rule is all you need to build lean muscle and keep insulin resistance at bay.
But let’s be honest: For anybody with an ounce of common sense, none of this should be a revelation.
Several doctors and health coaches on Twitter pointed this out to Dr. Attia, indicating they missed his bit at the end of the article.
My favorite response was from Dr. Mike Albert, who expanded on what everybody else has been saying:
- Exercise and Liraglutide (one of the earlier GLP-1 agonists) leads to better fat loss and superior body composition results compared to exercise, Liraglutide, or a low-calorie diet alone.
- Some researchers are attempting to use experimental muscle-sparing drugs like Bimagrumab in combination with Semaglutide to counteract muscle loss associated with rapid weight loss.
- Protein intake is likely best when you keep it at 2.4 grams per kilogram of bodyweight (or 1.0-1.1 grams per pound of bodyweight)
It’s important to keep all this in mind because if you look at the “lifestyle interventions” done alongside Semaglutide use in clinical trials, you’ll find they are far separated from my recommendations:
“Participants received individual counseling sessions every 4 weeks to help them adhere to a reduced-calorie diet (500-kcal deficit per day relative to the energy expenditure estimated at the time they underwent randomization) and increased physical activity (with 150 minutes per week of physical activity, such as walking, encouraged).
Both diet and activity were recorded daily in a diary or by use of a smartphone application or other tools and were reviewed during counseling sessions. Participants discontinuing treatment prematurely remained in the trial”
Fascinating what you can accomplish when you stick to what we’ve known about nutrition and bodybuilding for the past 100 years!
The T-Square Stack: Tirzepatide and Testosterone
I wanted to share something interesting I’ve discovered in treating nearly 2000 patients and counting with compounded Tirzepatide since June 2022.
In a lot of men who have a lot of visceral fat and desperately need to lose weight, there is always an incidence of low or suboptimal testosterone levels.
If you put those men on Tirzepatide for their weight loss, they will lose even MORE muscle mass compared to what they would have lost on a normal caloric deficit.
For that reason, I provide my patients with what I call “The T-Square Stack”: Tirzepatide in combination with therapeutic testosterone.
This allows my patients to maintain muscle mass, increase their energy levels, improve their insulin sensitivity, and achieve better body composition results.
Remember when I said I’d share a few tricks I’ve learned with using Semaglutide/Tirzepatide?
This is one of them provided free of charge. 😉
Myth #3: Semaglutide Has an Unfavorable Safety Profile

The only true way you’ll know if a medication has side effects is through its popularity and the real-world data we collect on it, i.e. how many people have used this medication and how long has it been out?
While it’s true that Big Pharma doesn’t always have our best interest in mind, the pharmaceutical-industrial complex is not entirely broken.
In the USA alone, we see an average of 4,500 drugs and devices pulled from the markets every year despite receiving full FDA approval.
So what’s the scoop on Semaglutide?
Let’s look at the loudest complaints people have echoed and see if they have any merit based on my own clinical experience and the available body of scientific evidence.
Dysgeusia
This is just a fancy medical term to describe an occurrence when otherwise pleasurable foods suddenly taste bad:
“[Patients] say the drug goes way beyond inducing extra satiety. They claim their favorite foods now actively taste bad.
This condition is called dysgeusia. It’s a change in the brain’s interpretation of what is going on in your mouth. Suddenly a Snickers bar could be acrid and sour. Or worse, you can’t taste the rainbow in a handful of Skittles.
This is a bummer on cheat day, but on the plus side, disdain for foods you normally crave, and overeat, will definitely help with weight loss.”
There’s also a clinical trial currently being run to get a more data-driven viewpoint on this phenomenon.
But I’m unconcerned about dysgeusia because I ultimately see this as a good thing.
I’ve even seen cases where patients will develop anhedonia (inability to experience pleasure) in response to food.
A lot of my patients will say “my only pleasure in life was food”, and my recommendation is to respectfully take pleasure in something else.
Celebrate the freedom of no longer being addicted to food or loving high-sugar desserts.
We should eat food for the sake of survival and better health.
Yes, it’s annoying, but that’s how you lose weight.
(NOTE: It takes a very experienced provider to help reframe this in a positive and motivating way that encourages long-lasting consistency with adherence to both Semaglutide and healthy lifestyle choices.
The way I talk to my readers is not the same way Dr. Eberwein will talk to his grossly overweight and obese patients).
There is even some early research (here and here) suggesting Semaglutide may reduce the amount of alcohol consumed and the frequency of alcohol consumption.
It wouldn’t surprise me if drinkers find themselves getting buzzed a lot quicker due to the gastric emptying that takes place.
“Ozempic Face”
This isn’t a medical term but it does describe a very common phenomenon I see happening in my patients.
The first instance I heard of this term was from New York dermatologist Dr. Paul Frank, who saw people on Semaglutide (Ozempic) undergo dramatic facial transformations to the point where they look older and more exhausted compared to what they looked like before using Semaglutide.
Unsurprisingly, he saw this phenomenon in a lot of his non-overweight rich patients.
He can now “tell” with 100% accuracy when someone is using Semaglutide because they’ll be skinny and need facial fillers for the first time in their lives.
But to describe what’s happening in more formal terms, this is generally a run-of-the-mill outcome with rapid weight loss:
“…when you maintain a higher weight for an extended period of time and then lose a large amount of that weight, the decrease in under-the-skin (subcutaneous) fat can lead to excess skin accumulation — especially in areas like the face, arms and abdomen.
It’s possible that you may see less excess skin if weight is lost in a controlled, gradual way…But some of it may just be inevitable.
Particularly as we get older, our skin and subcutaneous tissue is less able to adjust well to large changes in subcutaneous fat”
It’s yet another instance of how Mother Nature loves balance: A little bit of facial fat helps us have fewer wrinkles, while too much fat is equally unattractive and creates skin problems down the road.
At the same time, “Ozempic face” is just another testament to how successful Semaglutide is at eliminating fat.
You generally have a higher chance of “Ozempic face” if you’re in a situation where you only need to lose 15 pounds as your face ends up having lowered collagen production.
I try to minimize this outcome in my older patients by having them supplement with magnesium, amino acids and collagen while taking Semaglutide.
The good news is that you can easily treat an older-looking face if your bank account allows for it – more collagen supplementation, botox, microneedling, fillers, and so on.
However, for my more overweight patients, “Ozempic face” ends up being a good thing.
For patients who need to lose 40-60 pounds, they eliminate fat in the face, lower facial inflammation, and regain facial definition within the first 2-3 months.
Their physical appearance changes into what I would call a “cute Ozempic face” – cheekbones are visible again, their face starts to look more symmetrical, and triple chins turn into single chins.
In my professional opinion, the tradeoff of losing belly fat in exchange for needing to cosmetically fix your face (if you desire to do so) is more than worth it for your healthspan and lifespan.
Increased Heart Rate
While Semaglutide is not a stimulant like many weight loss drugs in the 1990s, I have rarely seen this happen in some of my patients who use Tirzepatide.
The good news is that Semaglutide and its prior predecessors do not elevate heart rate to the point of medical concern:
“All GLP-1RAs increase heart rate, and this is not different for semaglutide. In SUSTAIN 6, a placebo-corrected heart rate increase of 2.75 beats per minute (bpm) was observed for semaglutide 0.5 mg, and 3.2 bpm for the 1.0 mg dosage. This increase was not associated with adverse cardiac events.
In addition, no increase in cardiovascular outcomes were observed in SUSTAIN 6 and PIONEER 6, which is reassuring given the initial fear of adverse cardiac events with increased resting heart rates”
To try and prevent arrhythmia in some of my higher-risk patients (alongside constipation), I usually have them supplement magnesium while using Tirzepatide.
I wouldn’t worry about this as it is extremely unlikely to happen, plus I don’t believe we’ve fully fleshed out the mechanism of action to describe exactly how Semaglutide and other GLP-1 receptor agonists elevate heart rate.
“Unbearable” Nausea & Diarrhea
Many patients who are new to Semaglutide/Tirzepatide will describe a feeling of nausea within the first two days after their very first injection, OR they’ll experience it after they bump up their weekly dose to a higher amount.
This is completely normal in my experience – given that the half-life of both compounds is between 5-7 days, it makes sense why people would feel that way so quickly.
It’s all due to the drug decreasing appetite by delaying the speed of gastric emptying.
What I recommend to those patients is the following:
1 – Follow a “5-2” intermittent fasting diet where you eat normally 5 days out of the week and extremely low calorie (500-1000 calories) on 2 days of the week.
What my patients will do is allocate their two very-low-calorie days to the first two days after their initial injections.
2 – Eat as lean and clean as possible.
High protein, low carb and low fat is what I recommend so your food gets digested faster.
3 – Where permitted, switch from Semaglutide to Tirzepatide
There are a few patients of mine who cannot tolerate Semaglutide’s side effects but seem to do just fine on Tirzepatide.
I suspect this is because with Semaglutide there are six gradual increases in dose until you get to a maximally effective dose of 2.4 mg per week, whereas with Tirzepatide you only have one dose increase from 2.5 mg weekly to 5 mg weekly after a month.
Nausea and diarrhea are not rare with Semaglutide and Tirzepatide, but they are far more manageable through lifestyle modifications.
Acute Pancreatitis
This is not a “black box” warning per see, but it is a complication I have occasionally seen patients
The data we have so far suggests it is rare across all GLP-1 receptor agonists:
“Acute pancreatitis has occurred in patients treated with GLP-1 agonists. In trials, the incidence of acute pancreatitis in tirzepatide-treated patients was 0.23 cases per 100 patient-years compared to 0.11 cases per 100 patient-years in placebo-treated patients. If patients develop symptoms of pancreatitis (e.g. upper abdominal pain radiating to the back, nausea, vomiting), they should be evaluated promptly.
Patients with a history of pancreatitis were excluded from tirzepatide trials, so it is unknown if they are at greater risk.”
And although we still need to collect more data over several years, a pooled analysis of 7 large-scale cardiovascular outcome trials found no association between GLP-1 receptor agonist use and acute pancreatitis in patients with type 2 diabetes.
I’ve seen acute pancreatitis most prevalently with older GLP-1 receptor agonists… it’s possible with the newer agents (Semaglutide/Tirzepatide) but I haven’t seen any instances yet.
Unfortunately, having acute pancreatitis disqualifies you from Semaglutide use (there are blood tests you can do to diagnose acute pancreatitis if necessary).
I’ve even seen patients who take GLP-1 receptor agonists AND birth control pills at the same time, the latter of which may cause pancreatitis in rare instances.
As with any pharmaceutical drug, there are deal-breaking contraindications, so make sure you are evaluated by an experienced doctor BEFORE you use Semaglutide.
Sometimes you’re just shit out of luck and there’s nothing you can do about it.
Thyroid Issues
One final side effect I see people making too much fuss about is the possibility of developing thyroid cancer, one of the “black box” warnings that comes on the product information sheet of any GLP-1 receptor agonist.
For instance, here’s what you’ll see written for Tirzepatide:
“Data in animal studies has demonstrated the potential of developing medullary thyroid carcinoma. It is unknown whether this would also occur in humans at this time.
Given the theoretical risk, tirzepatide should be avoided in those with a personal or family history of medullary thyroid carcinoma. Patients with a history of MEN 2 (multiple endocrine neoplasia syndrome type-2) should also avoid tirzepatide.
Patients with other thyroid cancer-related risk factors should be advised of the theoretical risks.”
I’ll say this much:
We have 17 years worth of actual experience in using GLP-1 receptor agonists across many millions of diabetic patients without any reported increases in cancer that are significant enough to cause worry.
Even though there are newer drugs in this category, the mechanism of action and the side effects have always been the same (although the latter continues to improve with each successor drug).
If we had a high spike in thyroid cancer, it would be apparent by now and we would have shelved the GLP-1 approach to weight loss a very long time.
Now, one could make the reasonable argument that we don’t have the same abundance of data with GIP agonists as we do with GLP-1 agonists (in the case of Tirzepatide) and this would be a fair point.
While some studies contradict each other regarding the connection between GLP-1 receptor agonists and thyroid issues, this meta-analysis of 45 randomized controlled trials between 2009 and 2002 – testing everything between Exenatide and Semaglutide – reveals we still don’t know the answer:
” A total of 45 trials were included in the meta-analysis. Compared with placebo or other interventions, GLP-1 receptor agonists’ use showed an association with an increased risk of overall thyroid disorders (RR 1.28, 95% CI 1.03-1.60).
However, GLP-1 receptor agonists had no significant effects on the occurrence of thyroid cancer (RR 1.30, 95% CI 0.86-1.97), hyperthyroidism (RR 1.19, 95% CI 0.61-2.35), hypothyroidism (RR 1.22, 95% CI 0.80-1.87), thyroiditis (RR 1.83, 95% CI 0.51-6.57), thyroid mass (RR 1.17, 95% CI 0.43-3.20), and goiter (RR 1.17, 95% CI 0.74-1.86).”
But then it concludes:
“GLP-1 receptor agonists did not increase or decrease the risk of thyroid cancer, hyperthyroidism, hypothyroidism, thyroiditis, thyroid mass and goiter. However, due to the low incidence of these diseases, these findings need to be examined further.”
There were several contradictory findings in the meta-analysis, which really goes to show we have a lot to figure out (for example, risks of overall thyroid disorders were higher with Liraglutide and Dulaglutide but not the newer GLP-1 receptor agonists).
However, even with all this being true, I would argue the ultra-small risk of thyroid cancer is significantly outweighed by the health benefits of treating obesity and insulin resistance in relation to cardiovascular disease and other cancers.
But just like acute pancreatitis, there are some people with pre-existing thyroid problems who are not allowed to be prescribed Tirzepatide.
I even had one patient come in with her whole thyroid removed due to thyroid cancer… yes, the thyroid is gone, but GLP-1 receptor agonists haven’t been studied in people with removed thyroid and it’s possible she may have had leftover thyroid cells.
Not worth the risk for me.
As a side note, some studies suggest Tylenol may increase liver cancer risk but that doesn’t stop people from using it!
Myth #4: Semaglutide Should Be Used By Children

At the start of the year, there was a social media uproar over an article AP News posted about the American Academy of Pediatrics’ update to their guidelines on treating obesity.
“For the first time, the group’s guidance sets ages at which kids and teens should be offered medical treatments such as drugs and surgery — in addition to intensive diet, exercise and other behavior and lifestyle interventions
“In general, doctors should offer adolescents 12 and older who have obesity access to appropriate drugs and teens 13 and older with severe obesity referrals for weight-loss surgery, though situations may vary.
“The guidelines come as new drug treatments for obesity in kids have emerged, including approval late last month of Wegovy, a weekly injection, for use in children ages 12 and older. Different doses of the drug, called semaglutide, are also used under different names to treat diabetes.
A recent study published in the New England Journal of Medicine found that Wegovy, made by Novo Nordisk, helped teens reduce their BMI by about 16% on average, better than the results in adults.”
A brief look on Twitter will show you that people are NOT happy with this announcement.
“You’re shilling for Big Pharma and you should burn in hell!”
“Have you heard of something called DIET and EXERCISE?”
“DO you even know what they’re feeding kids at school lunches?”
Well, at the expense of having the online mob come after me… I view this announcement as a godsend and I will happily use this drug for younger teens where I feel it is appropriate.
Look, at the end of the day, insulin resistance affects us all the same.
When a child already has developed metabolic syndrome, you effectively have an adult’s metabolic problems and it’s exactly why type 2 diabetes in pediatric patients sees around 5,000 NEW cases per year.
OBVIOUSLY, the best time to teach young children the importance of healthy lifestyle habits was yesterday.
The second best time is right now, and unfortunately, we are at a point where we have to weigh out all the benefits and risks.
We already know the long-term downstream effects of insulin resistance created by high sugar consumption towards obesity, cancer and disease.
As a functional medicine practitioner, I can say Tirzepatide – once approved in adolescents – will be the best tool we have for treating insulin resistance in younger patients.
I would much prefer it over gastric bypass, which is already happening in teenagers.
But remember what I said about Semaglutide/Tirzepatide in the context of lean muscle loss: It is ONE tool meant to be used alongside other tools, and it can never be used at the expense of lifestyle factors.
Myth #5: Semaglutide is Meant to Replace Healthy Lifestyle Habits

One major criticism of Semaglutide and the other GLP-1 receptor agonists — any weight loss drug, really — is the weight regain once you stop using the drug.
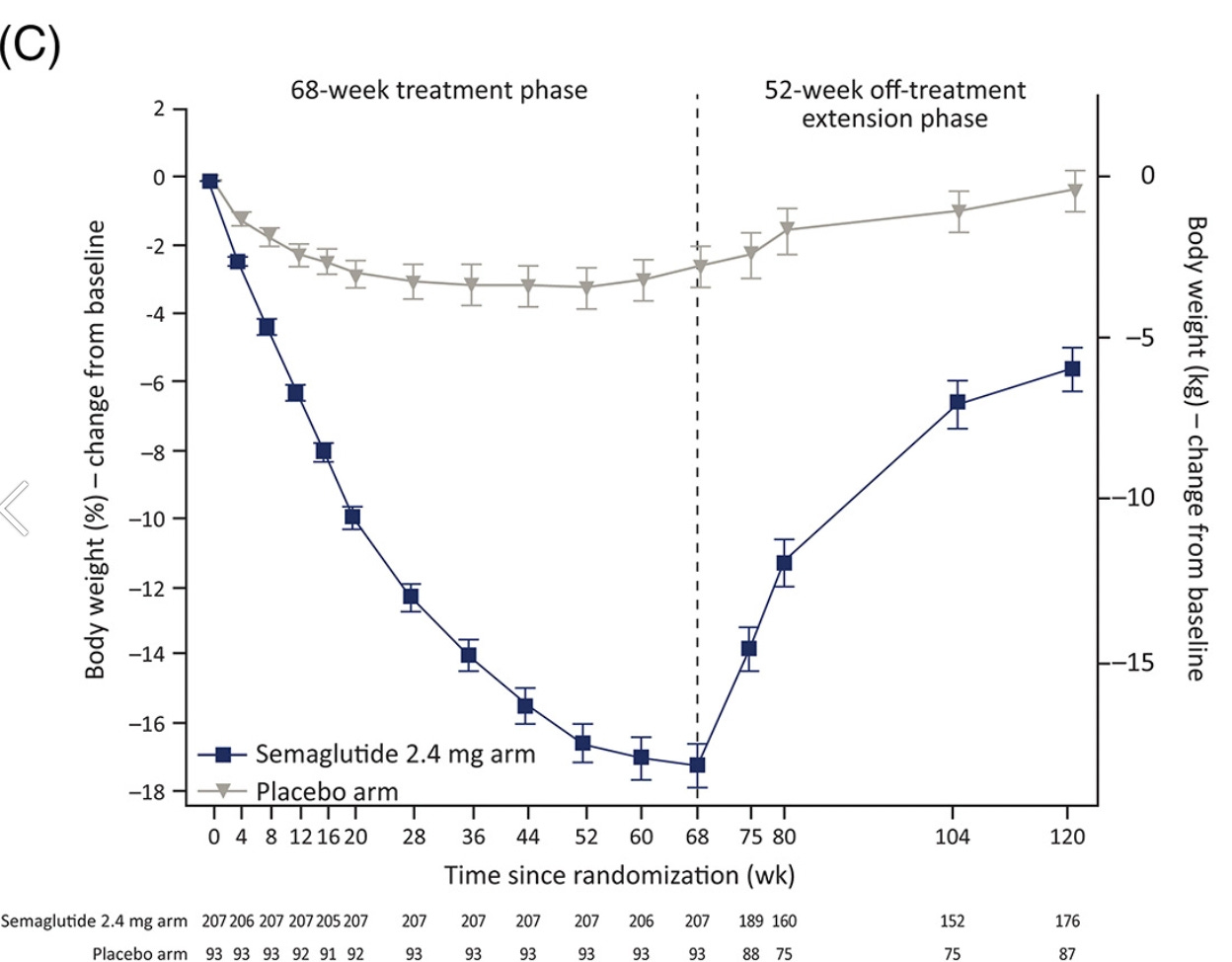
A popular study quote to “take down” Semaglutide is a follow-up of the STEP-1 trial, where patients who received Semaglutide or placebo would discontinue all treatments for 52 weeks (adding up to 120 weeks total).
Here’s what you’ll find in the abstract:
“STEP 1 (NCT03548935) randomized 1961 adults with a body mass index ≥ 30 kg/m2 (or ≥ 27 kg/m2 with ≥ 1 weight-related co-morbidity) without diabetes to 68 weeks of once-weekly subcutaneous semaglutide 2.4 mg (including 16 weeks of dose escalation) or placebo, as an adjunct to lifestyle intervention. At week 68, treatments (including lifestyle intervention) were discontinued.”
“One year after withdrawal of once-weekly subcutaneous semaglutide 2.4 mg and lifestyle intervention, participants regained two-thirds of their prior weight loss, with similar changes in cardiometabolic variables.”
And when people share this information, expect them to share this image from the study to make their point:
Checkmate, right?
WRONG!
If you don’t read the study carefully, you’ll get the false impression that Semaglutide was stopped, people tried to stick to exercise and healthy dieting, yet gained back the weight anyways.
Read the abstract closely… it says “withdrawal of once-weekly subcutaneous semaglutide 2.4 mg AND lifestyle intervention”
What did people think was going to happen?
I need to emphasize again that drugs like Semaglutide and Tirzepatide are PART of a multidisciplinary approach — my patients also eat a high-protein diet, exercise frequently with weights, take additional supplementation if needed, and change their mindset to guarantee long-term success.
People either misinterpret this study and say Semaglutide is completely useless, or vouch for Semaglutide so hard to the point where they claim it’s absolutely impossible to lose weight without it.
This battling of opposite views is very apparent in a quote I found from a doctor on Substack:
“The longer you can stay at your lower ideal weight, the easier it is to maintain. And the more leeway you have to veer from your diet here and there on special occasions. But you have to more or less stick to it. And understand that you have an underlying metabolic condition you’re treating. If you didn’t have the condition, you wouldn’t have been overweight in the first place.
But here is the kicker. The pharmaceutical industry wants you to believe long-term weight loss maintenance is an unachievable goal for most people. Obesity is a disease. And, as such, it should be treated with drugs.”
Let me dispel this debate once and for all with my hard-won perspective after treating thousands of patients over nearly two decades.
There’s a saying in medicine that “genetics loads the gun but environment loads the trigger”, meaning that genetics has a lot to do with weight loss success but it doesn’t mean you have to spend the rest of your life on pharmaceutical drugs.
By the time my patients lose 40-60 pounds of fat and are finally ready to stop using Semaglutide/Tirzepatide, their biochemistry has completely changed.
Chronic inflammation is lowered, levels of leptin and ghrelin are restored to normal, they can feel full on protein and veggies instead of Coke and cookies, healthy habits have been installed to the point of replacing unhealthy habits… the patient is physically and psychologically a completely different person.
Sure, they may gain 10-20% of their bodyweight back due to a rebound effect, but their new habits allow them to minimize the damage and in many cases that last 10-20% of bodyweight gets lost anyways.
But none of this would be possible if I wasn’t helping my patients consistently make new lifestyle choice WHILE using Semaglutide and not AFTER using the drug.
And yes, a rare few people may need to stay on Semaglutide/Tirzepatide for life… they are the exception and not the rule.
Myth #6: Semaglutide is Another Evil “Big Pharma” Ploy

This is similar to the first myth I tackled but I want to take a different angle here.
There has also been a lot of uproar about celebrities who are getting paid by Novo Nordisk (the manufacturer of Semaglutide) to promote the benefits of the drug:
Weight loss pharma is hiring celebrities to go on tour so they can tell fat people it’s not their fault, that they can’t fix themselves, and that they have the pharmaceutical cure.@IAMQUEENLATIFAH is a complete hypocrite and sell outhttps://t.co/qgLzvJBjeV pic.twitter.com/8JDFMuam16
— Alan Roberts (@TheMFingCOO) June 18, 2022
That, and the standard practice of doctors receiving financial kickbacks in exchange for speaking positively about Semaglutide (obviously this did NOT sit well with people)!
I think a lot of the outrage and finger-wagging comes down to a lack of clearly defined boundaries about what is and isn’t acceptable.
For example, we have someone like Rosie O’Donnell who announced in January 2023 that she was using Tirzepatide for weight loss, was down 10 pounds and no longer had intrusive thoughts about food (and is now considering bumping her weekly dose up after hitting a plateau).
In her context, I’m not opposed to her promoting Tirzepatide.
Someone who fights obesity KNOWS what to do, but it’s the irrational hunger caused by disregulated levels of leptin and ghrelin that drives them crazy.
Tirzepatide decreases and uncouples the dopamine release from food so people no longer find “bad foods” so pleasurable, thus bringing them a level of mental freedom they never had before.
However, I would be opposed to someone who was getting kickbacks – doctor or celebrity – to say that Semaglutide/Tirzepatide can be used by people who want to lose 10-15 pounds of stubborn body fat.
If we are honest about what these drugs can and can’t do, and how to use them properly in the context of lifestyle habits, I am more than excited by any efforts we can make to get these drugs into more people’s hands.
I take on the perspective that “Big Pharma” has its positive upsides but greed leads to a lot of unnecessary mistakes.
Likewise, I believe the majority of doctors and researchers have the best intentions in their heart.
I have no problem using pharmaceutical drugs as a traditionally-trained doctor, but I can use my clinical training and knowledge of functional medicine to know what their role is in the context of overall health.
In my opinion, the best approach is to combine what’s good from both functional medicine and Big Pharma in order to get the most optimal results.
I’ll end with this final hot take: As much as we need to criticize and watch Big Pharma like a hawk, at some point we need to start taking personal responsibility for our own lives.
“Big Pharma” did not grow into the monstrosity it is today all by itself… American society has allowed it to fester a reputation of corruption and “profits over health” because we do not do our part to become healthy.
If you’re ranting against the evils of the pharmaceutical industry while eating out at McDonalds, then you are the reason why they continue to exist.
Until we recognize how our actions and daily habits contribute to the existence of Big Pharma, they will take full advantage of the problems we often create for ourselves.
CONCLUSION: GLP-1 Receptor Agonists are Here to Stay!

One of the reasons why I love Dr. Eberwein’s perspective on weight loss is because he truly practices what he preaches.
He introduced me to Semaglutide in December 2021 and gave me the heads-up on Tirzepatide in August of 2022 before they truly reached mainstream consciousness… and both drugs completely changed how I perceive the problem of weight loss.
<And wait until you see how I cover them in my soon to be released book 30 Days 2 Shredz due out late April of this year>
Even as a fully optimized individual, the dramatic reduction in appetite I experienced gave me more sympathy toward obese folks and helped me better understand their mental struggle in losing weight.
And although I may disagree with Dr. Eberwein on some of the things he said here, I know they come from a place of real-world experience and a genuine desire to rid the world of chronic disease.
Semaglutide and Tirzepatide may not be available for purchase due to their status as prescription drugs, but many more effective fat loss peptides are available right now at Limitless Life Nootropics.
Use code JAY15 at the checkout cart for 15% off!
I also talk about both weight loss peptides in deeper levels in my newest book Optimize Your Health with Therapeutic Peptides, now the #1 best-selling book on Amazon for peptides and sitting at 180 reviews with a 5.0 score!
But if you REALLY want me to hand-hold your way through the wonderful world of peptides and save money at the same time…
…grab a FREE copy of my eBook Top 10 Mistakes People Make When Starting Therapeutic Peptides!
You’ll be signed up for an email sequence where I’ve hidden a HALF-OFF coupon code for my premium Therapeutic Peptides Course that constantly receives new intel updates I will never publish to the public.
As always…
Raise Your Vibration To Optimize Your Love Creation!
PS – Want access to private interviews I’ve done with world-class physicians like Dr. Eberwein that will never make it to my podcast?
If so, join The Fully Optimized Health Private Membership Group.
It’s your greatest opportunity to fully optimize your health and gain total access to me and my network of high-level men and women living their highest and best life.